Market access remains one of the most complex links in the pharmaceutical value chain, and studies show it has grown in complexity significantly in recent years. The advent and widespread adoption of new digital technologies is changing expectations from patients, practitioners, and payers, while fluctuating and novel market pressures make it difficult to devise useful strategies.
Artificial intelligence (AI) is the most appropriate tool for cutting through this complexity and making data-driven market access decisions. An unprecedented quantity of data is now available to pharma providers, and those with the tools and knowledge to make use of it will quickly pull ahead.
This article examines some of the current challenges to market access and how AI can help solve them.
Current Challenges to Market Access
Pharmaceutical companies face a variety of challenges when it comes to bringing new drugs to market and ensuring the continued purchase of existing ones.
Rising pressure regarding pricing and reimbursement. On multiple fronts, pharmaceutical companies are being pressured to reduce prices. Healthcare costs continue to rise due to aging populations, an increased prevalence of chronic illnesses, and more expensive therapies. As a result, pharmaceutical companies are facing ever stricter pricing and reimbursement tools, like reference pricing and generic substitution, as well as steeper clawbacks.
At the same time, the influence of payers (e.g. PBMs) continues to grow, resulting in higher and more frequent rebates (that don’t always make their way to pharmacies and payers), accompanied by a staggering rise in formulary exclusions in the last half-decade. Finally, reimbursement plans are shifting from traditional fee-for-service to value-based and patient outcome measures, which means greater pressure to collect as much and as granular data as possible, rapidly analyze it, and spin it into a coherent, compelling story.
Expectations from practitioners, payers, and patients are rapidly changing. Today’s stakeholders are fed up with antiquated barriers to accessing pharmaceutical reps and drug information. In fact, according to one study of 189 U.S. P&T committee members making formulary decisions at hospitals, IDNs, PBMs, MCOs and ACOs, “44% of P&T committee members said they would use pharma digital resources more frequently if pharmas made it easier to find content dedicated to formulary decision makers” like trend reports for disease areas or interactive budget modelling features. Pharma needs to focus on distilling complex data into easy-to-use, easy-to-understand digital content.
As for patients, their “involvement and partnership is now an essential and necessary component of the drug development process” necessary to “meet the demands of regulatory and reimbursement authorities” and “deliver new products which meet the expressed needs of patients for which they are intended” (Holtorf & Cook, 2018).
Stakeholder fragmentation. Finally, there exists today a broader range of market access stakeholders than ever before, and greater complexity in both global and regional market access. Market access teams need to be able to make convincing, data-driven, outcome-based pitches to a wide variety of individuals and bodies, each with their own expectations and agendas, within ever tighter timeframes.
The common thread to all of these challenges is that market access teams need more accurate and more granular data that’s broader in scope and provenance, with faster insights that are easier to personalize and convey to a variety of stakeholders. The answer to all these requirements lies in artificial intelligence (AI).
AI Solutions for Market Access
The main goal of market access teams is to achieve the broadest possible payer access with the best possible margins and the most advantageous reimbursement scheme. A tall order, no doubt, especially given the challenges mentioned above. Fortunately, there are a variety of AI tools available today to help teams do just that.
Pricing
Pricing is an important but highly complex element in market access. It involves analyzing large amounts of data from ever more diverse sources—something AI excels at. Rather than spending hours pouring over clinical trial and real-world data (RWD), past drug submissions and evaluations, and global, regional, and historical pricing data, market access teams can simply feed this data into an appropriately structured AI system for fast results, largely free from human error and easily translatable into relevant, compelling insights.
Several AI-powered companies exist that enable value-based pricing that has demonstrated up to 90% accuracy. Accurate predictive pricing enables pharma companies to better adjust their approach to approval and reimbursement, while the ability to use and intelligently analyze ever more data from patient outcomes and clinical trials allows for value-based pricing that appeals to payers, all while providing maximum profits.
This type of AI-powered technology assisting market access and pricing professionals to predict the performance of any new molecule years in advance. This also provides them with a more thorough understanding of the driving factors that influence the final outcome enabling better decisions as well as providing strong data-driven bases for negotiations.
An article by the Professional Society for Health Economics and Outcomes Research (ISPOR) highlights five different domains with high opportunity for impact from AI, all of which relate to pricing.
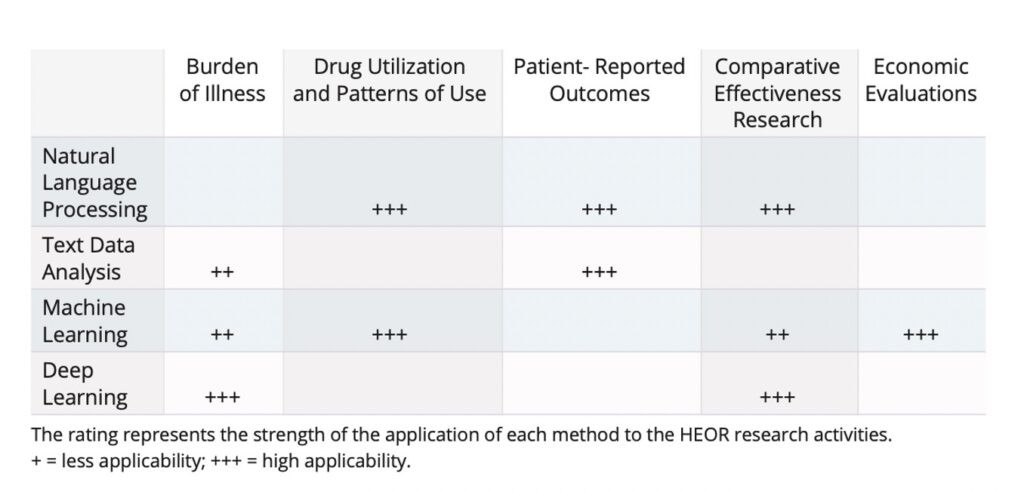
Rueda, Cristancho & Slejko (ISPOR). “Is Artificial Intelligence the Next Big Thing in Health Economics and Outcomes Research?”
Reimbursement
Outcome-based contracts (OBC) and value-based models or “value pricing” are promising approaches to pricing and reimbursement but require rapid analysis of large amounts of data to ensure advantageous reimbursement tiers are approved as quickly as possible and that providers aren’t left holding the bag when expectations aren’t met. AI can assist by better identifying qualifying populations with greater certainty around efficacy, informing manufacturers on where OBCs are most likely to be advantageous, and, of course, tracking and analyzing outcomes. By using advanced analytics from structured and unstructured patient data one can have faster, more accurate insights for both payers and providers.
Field reimbursement managers (FRMs) work on the frontlines of reimbursement. Given the complexity of their role, they are also uniquely well positioned to benefit from AI solutions. Tools exist that can be used to proactively intervene on behalf of patients who are likely to experience roadblocks in their journey—before the roadblocks occur – leading to swifter resolutions and more successful interventions for patients at risk of discontinuation, ultimately leading to better patient care (and outcomes).
Indeed, there are a number of ways AI can be used for simpler, faster reimbursement.
Stakeholder Engagement
Finally, pharmaceutical companies must engage more effectively with practitioners and patients. One way to do this is by leveraging AI to engage stakeholders across multiple channels and in a fashion that facilitates rather than impedes the free exchange of critical pharmaceutical and biomedical information. Digital tools that meet payers’ and others’ information needs, for example, powered by AI and accessing fully-compliant healthcare and drug data, make life easier for formulary decision-makers. In fact, 52% of P&T committee members from a recent survey agree that interactive content “makes meetings with pharma account managers more valuable.” And managing the data—and gaining insights from it—on all these stakeholders is another job perfectly suited to AI.
AI can also provide pharmaceutical companies with precious insights not only into patients and practitioners but also payers. Product presentations must be done with the right message, in the right language, and at the right time for a variety of stakeholders and audiences whose needs and expectations may vary widely. With the right AI strategy, for example, businesses can develop submission documents based on drivers specific to a given formulary, with optimized language according to previous successful submissions.
Conclusion
The challenges companies and actors face in market access today are significant, and only growing in complexity. Fortunately, artificial intelligence is a powerful, adaptable tool that pharmaceutical companies and their partners can use to improve market access.
Found this article interesting?
If you’re looking for help on creating an AI powered market access for supercharged results, speak with us.
For more information, contact Dr Andree Bates abates@eularis.com.